Oropouche fever has emerged as a significant public health concern, particularly for pregnant women in Brazil. This mosquito-borne virus poses severe risks during pregnancy, including potential fetal complications associated with vertical transmission of the Oropouche virus. Recent studies indicate alarming statistics, with confirmed cases revealing impacts on maternal health in Espírito Santo State. Notably, among the 73 pregnancies analyzed, there was one spontaneous abortion and several documented cases of adverse fetal outcomes. Understanding the implications of Oropouche fever during pregnancy is crucial for developing effective health strategies that can mitigate risks associated with this reemerging disease.
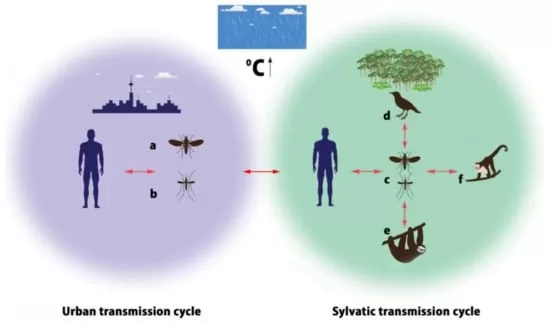
Referred to in various terms, the Oropouche virus represents a growing threat to maternal and fetal wellbeing. As a tropical vector-borne disease, it raises urgent questions regarding its effects during pregnancy, particularly in endemic regions like Brazil. The transmission of the Oropouche virus from mother to fetus, often referred to as vertical transmission, can lead to significant complications for developing embryos. Research has increasingly focused on maternal health implications and the challenges posed by this fever in pregnancy. By delving into the complexities surrounding Oropouche fever, we can better comprehend its extensive impacts on both mothers and their unborn children.
Understanding Oropouche Fever: An Overview
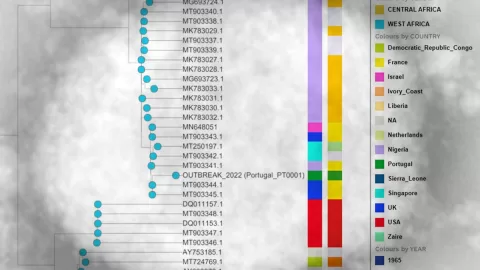
Oropouche fever is a viral illness transmitted primarily by mosquitoes, prominent in tropical regions, particularly in South America. This disease has resurfaced as a significant public health concern, especially in Brazil, where recent outbreaks have raised alarms among health officials and pregnant women alike. The Oropouche virus, belonging to the Orthobunyavirus genus, leads to symptoms that are often mistaken for other febrile illnesses, complicating its diagnosis. High incidence rates reported in Espírito Santo necessitate immediate awareness and education surrounding the implications of the virus, particularly for vulnerable populations.
The complexities of Oropouche fever are magnified during pregnancy, as the physiological changes in a woman’s body make them more susceptible to infections. The clinical manifestations of the disease can vary, and symptoms like severe headaches, fever, and joint pains can impede a woman’s overall health, possibly affecting her maternal responsibilities. As healthcare systems adapt to respond to this emerging threat, understanding the epidemiological patterns of Oropouche fever will be crucial in formulating effective healthcare strategies.
Maternal Health Challenges During Oropouche Fever
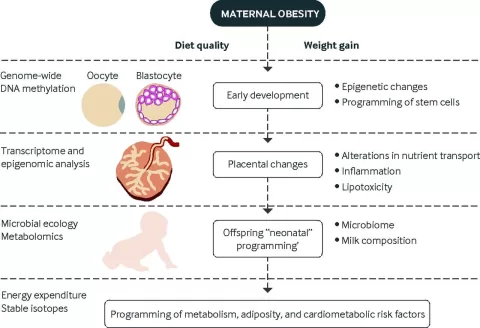
Pregnancy presents a unique set of challenges, and the emergence of Oropouche fever exacerbates these difficulties. Maternal health in Brazil is facing multifaceted challenges, especially with diseases like Oropouche fever. Data from recent studies indicate that pregnant women infected with the virus not only experience the direct effects of the disease but also face heightened risks of complications such as spontaneous abortion and fetal developmental issues. This reality emphasizes the urgent need for integrated maternal healthcare services that take into account the risks posed by emerging infectious diseases.
Oropouche fever’s potential for vertical transmission necessitates close monitoring and intervention in maternal health practices. With five cases of positive placental tests for the Oropouche virus in pregnant women, it’s clear that the effects of this virus can be profound, leading to serious fetal complications. Health practitioners must ensure that women who exhibit symptoms are closely monitored, and effective preventive measures, such as vector control strategies, are implemented to protect maternal and fetal health.
Fetal Complications Associated with Oropouche Fever
The repercussions of Oropouche fever extend beyond the immediate symptoms experienced by the mother, significantly impacting fetal health. Emerging evidence suggests that infections during critical periods of pregnancy, particularly in the first and third trimesters, can lead to severe fetal complications. In the analyzed data, the incidence of spontaneous abortion among the cases studied reinforces the urgent need for awareness regarding the potential teratogenic impacts of the Oropouche virus.
Furthermore, studies exploring the correlation between Oropouche virus and fetal malformations present concerning findings. Complications, including low birth weight and developmental delays, signal the importance of specialized care and monitoring for pregnancies complicated by viral infections. Continuous research efforts are vital to ascertain the full extent of Oropouche fever impacts on fetal development, thus equipping healthcare providers with the necessary knowledge to support affected families.
Vertical Transmission of Oropouche Virus
The concept of vertical transmission of the Oropouche virus is a critical concern in obstetrics, particularly for regions where the disease is endemic. Evidence suggests that not only can the virus affect pregnant women, but there is also a risk that it can be passed onto their fetuses during pregnancy. This possibility prompts a demand for rigorous screening protocols and research to understand the mechanisms and frequency of vertical transmission related to Oropouche virus.
Understanding the dynamics of vertical transmission can help inform preventive strategies to mitigate risks for both mothers and their unborn children. Implementing effective vector control measures and maintaining heightened surveillance in pregnant populations can play an essential role in reducing the incidence of Oropouche fever and its subsequent fetal complications. Health policymakers must prioritize research efforts that delve deeper into these transmission pathways to create robust maternal health frameworks.
Preventive Strategies for Oropouche Fever in Pregnancy
Given the serious implications of Oropouche fever for maternal health and fetal development, it is imperative to establish effective preventive strategies. Public health initiatives in Brazil should focus on educating pregnant women about the risks associated with Oropouche fever, including common symptoms and preventive measures. Community-centered health campaigns can enhance awareness of vector control methods to minimize mosquito exposure, which is critical in endemic regions.
Moreover, healthcare providers should integrate Oropouche fever into differential diagnosis protocols for pregnant patients exhibiting febrile illnesses. By honing in on prompt diagnosis and management strategies, healthcare services can improve outcomes for mothers and their infants. This can include comprehensive prenatal care that ensures all pregnant women are educated about potential risks and have access to appropriate interventions if they experience symptoms.
Impacts of Oropouche Virus on Maternal Health in Brazil
The resurgence of Oropouche virus poses significant challenges not only for individual health but also for public health systems across Brazil. Maternal health issues can be exacerbated by the complexities introduced by viral infections like Oropouche fever. Pregnant women, particularly in Brazil’s vulnerable regions, require specialized care that addresses the potential risks posed by such diseases, including a higher prevalence of underlying health conditions such as hypertension and diabetes.
Data collection from localized outbreaks shows that many pregnant women within the age range of 20-39 exhibit pronounced symptoms, indicating that targeted healthcare strategies are necessary. Enhancing maternal health protocols to include robust monitoring for Oropouche fever can assist in preemptively addressing complications and safeguarding the health of both the mother and the fetus.
Healthcare Protocols for Managing Oropouche Fever in Pregnancy
To effectively address the risks associated with Oropouche fever in pregnancy, established healthcare protocols must be adapted to include the latest findings on the virus and its complications. This involves not only recognizing the symptoms of Oropouche fever but also understanding its potential impacts on maternal and fetal health. Enhanced training for healthcare workers regarding the identification and management of infected pregnant women will be critical in reducing adverse health outcomes.
Additionally, collaboration among health sectors can facilitate comprehensive care solutions for pregnant women exposed to the Oropouche virus. Development of clinical guidelines that emphasize rapid diagnostic testing and treatment pathways for Oropouche fever will significantly improve maternal health outcomes. An urgent response system for cases identified during pregnancy could also contribute to minimizing the risks associated with both maternal and fetal health.
Research Necessity for Oropouche Fever and Maternal Health
Increasing the understanding of Oropouche fever’s implications for maternal and fetal health is crucial for developing effective public health policies. Further research is warranted to explore the links between the Oropouche virus and various maternal and fetal complications, emphasizing a need for longitudinal studies that assess long-term outcomes post-infection. Such data can illuminate the teratogenic nature of the virus, driving targeted interventions aimed at safeguarding pregnant women.
Engagement with academic institutions and public health organizations can contribute to a robust body of evidence regarding Oropouche fever. As ongoing research continues, it is essential to disseminate findings widely to equip healthcare providers, patients, and community leaders with the knowledge to respond proactively to potential outbreaks. Establishing a research agenda focused on understanding the full spectrum of Oropouche fever impacts can be a game-changer for maternal health in Brazil.
Addressing the Societal Impacts of Oropouche Fever
The societal implications of Oropouche fever extend beyond the biomedical context, influencing public perceptions and healthcare access among pregnant women. The fear surrounding viral infections can lead to increased anxiety among expectant mothers, which in turn can affect maternal health outcomes. Addressing these psychological impacts is essential, and community support systems must be strengthened to provide reassurance and education regarding Oropouche fever.
Moreover, community engagement initiatives can play a pivotal role in alleviating societal burdens associated with the disease. By promoting local partnerships that focus on both awareness and prevention of Oropouche fever, long-term strategies can be cultivated to mitigate the risks for pregnant women and their families, fostering a healthier future generation free from the developmental hindrances associated with Oropouche virus.
Frequently Asked Questions
What are the maternal health risks associated with Oropouche fever during pregnancy?
Oropouche fever poses significant risks to maternal health during pregnancy, particularly in the first and third trimesters. Symptoms of the virus might lead to severe complications, including an increased risk of spontaneous abortion and hypertension-related issues. Pregnant women experiencing fever and Oropouche symptoms should seek medical evaluation immediately.
Can Oropouche fever lead to fetal complications during pregnancy?
Yes, Oropouche fever can lead to various fetal complications. In a study conducted in Espírito Santo, Brazil, spontaneous abortion and poor fetal development were noted among cases of pregnant women infected with the virus. Vertical transmission of the Oropouche virus may also result in teratogenic effects on the developing fetus.
What is vertical transmission of Oropouche fever and its implications for maternal health?
Vertical transmission of Oropouche fever refers to the transfer of the virus from a pregnant mother to her fetus during pregnancy. This can lead to severe implications for maternal health, including increased risks of fetal malformations and complications in pregnancies affected by the virus. Ongoing surveillance and research are required to understand these risks better.
How does Oropouche fever impact pregnancies in endemic regions like Brazil?
In endemic regions such as Brazil, Oropouche fever significantly affects pregnancies, presenting challenges such as elevated incidence of maternal health complications, spontaneous abortions, and developmental issues in fetuses. Reports highlighted the need for enhanced diagnostic protocols for pregnant women displaying fever symptoms to mitigate these risks.
What are the recommended strategies for managing Oropouche fever in pregnant women?
It is vital to integrate Oropouche fever into differential diagnosis protocols for pregnant women presenting with fever and related symptoms. Additionally, vector control strategies, symptomatic treatments, and enhanced medical evaluations post-infection are essential for managing maternal health and preventing complications associated with the virus.
| Key Point | Details |
|---|---|
| Synopsis | Study on Oropouche fever exploring risks in 73 pregnancies, noting live births and spontaneous abortion. |
| Methods | Epidemiological assessments through RT-PCR testing among symptomatic pregnant women. |
| Results | 4,062 reported cases; complications included spontaneous abortion and fetal impacts. |
| Discussion | Need for better monitoring protocols and preventive measures for pregnant women. |
| Conclusion | Oropouche fever significantly impacts maternal and fetal health; urgent preventive action is required. |
Summary
Oropouche fever poses significant risks to both maternal and fetal health, as highlighted by the analysis of 73 pregnancies in Espírito Santo State, Brazil. The study found concerning links between the virus and adverse pregnancy outcomes, including spontaneous abortion and malformations. Enhanced surveillance, monitoring protocols, and preventive measures are crucial to mitigate the impacts of this virus, especially among pregnant women in endemic areas.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.